When we plan for our inevitable death, we can make our end of life easier for our loved ones.
In this Episode:
What Barriers Keep us From Completing an Advance Directive?
Even though people say they are prepared to die, no one truly is. And how can we be?
It’s like being strapped into the largest roller coaster in the world and being asked if you are ready to ride. Well, yes. And no. But the ride is starting anyway and it’s too late to get off. So, you can white knuckle it and scream, or raise your arms over your head and enjoy yourself, but either way, you are taking the ride.

In this episode Marianne talks about how the unknown of it all can leave us with waffling. Maybe, like the mother in the NYT article titled “I Asked My Mom if She Was Prepared to Die”. Mom answered the question in this way, “Not really. But I am prepared with my paperwork”.
We have shared several podcasts and resources to get you started. Please see the resources and related content below. Don’t let yourself or your family get caught off-guard and take care of these things ahead of time.
FAQ on Advance Care Planning
- What is advance care planning (ACP)? ACP is a process that helps families and health care practitioners respect a person’s values and priorities about their care at the end of life.
- Why is ACP important? There is an increase of chronic diseases, an growth in life expectancy, and increasing attention paid to the decisional autonomy that makes ACP an important part of care at the end of life.
- What is an important aspect of ACP? Communication between the person, family, and the medical staff that will take care of him/her. ACP helps to ensure that the important aspects of end-of-life care are thought about in advance and documented.
Need Ideas of What to Put in Your Advance Care Planning? Here’s an Example
Charlie shared a letter written by a friend of Marianne’s that is a wonderful example of what one may want to include in your own advance directive. It is a combination of very specific considerations of his wishes, but also things that not many may think about including for comfort measures. Take a look and see if it gives you any ideas. These instructions will not be right for everyone. What would you change to make it work for you?
Over the past two weeks, my wife and I made several trips to visit her 83-year-old father who was in an ICU three hours away with pneumonia and sepsis. Last week, after multiple family discussions, we all agreed to move him to a nursing facility on hospice, where he died peacefully the next day. The day after that, my previously healthy 89-year-old father fell in his backyard, hitting his head on a brick walk. A few hours later, he was on a ventilator (again, about a three-hour drive from our home) with a hematoma in his neck that was compressing his airway. After 72 scary hours, he has been extubated and is doing well at present. When I got back home last night, I wrote this letter to my wife and two daughters.
Dear girls—
With grandpa’s death last week and my dad’s current hospital stay, I am reminded that death is always near, so it seems proper to make what plans one can. As you know, I have talked about much of this before and filled out some forms, but here it is in more detail.
If I am very ill and cannot communicate my wishes
1. First, make sure communication efforts are pursued with adequate energy and diligence. Persons who are critically ill but who still have cognitive capacity and decision-making ability are sometimes not addressed directly because it seems too difficult or uncertain to get through, or because of wishes (understandable but misguided, I think) to spare them mental stress. One of my fears of being on a ventilator is not being able to convey my wishes, such as “my nose itches” or “my feet are cold” or “make that machine stop beeping” or “tell me my condition and prognosis as clearly and completely as you can.”
I’m pretty sure hearing someone say “it’s not your time” or “we’re not going to let you go” would not be comforting or helpful to me.
I might be groggy or confused, so orienting statements (where I am, what day it is, how I got there) and repetition are useful.
2. Please make sure my comfort is aggressively optimized.
a. Ask me if I have pain and if I want something for that. If I do, ask the nurse to treat it. If there are barriers, be polite but persistent. In most cases, “Can you please contact the physician?” will get as quick a response as “I have a sharp object in my purse and I will use it,” and it is less likely to lead to subsequent complications and delays.
b. I would like to listen to music of my liking. Good choices for me include Beatles, Coldplay, TMBG, Elliott Smith, The Decembrists, Bach, and Beethoven. (There’s a playlist on my iPhone entitled If I’m Sick.) It’s possible I would like some selections of C&W, disco, or hip-hop, but why take a chance?
c. Please avoid or minimize the use of restraints. Occasionally those are necessary to prevent a delirious patient from pulling out tubes, but they are potentially dangerous and antithetical to comfort. Even if required, they can generally be removed while someone is present who can ensure that the patient does not pull on the wrong thing. If the nurse objects, be polite but persistent. (Just in case, keep a sharp object in your purse.)
What does that mean [for an intervention to “help”]?
I define it thus: “get me to a point where I can enjoy life and interact meaningfully with loved ones.”
3. Regarding the use of life-sustaining interventions, I want the same thing that most people want: if a particular intervention is reasonably likely to help, use it, but not otherwise. Of course, there are two tricky parts to this expression—
a. “…help…” What does that mean? For this context, I define it thus: “get me to a point where I can enjoy life and interact meaningfully with loved ones.” I’m sure you recognize this is different from “keep me alive.”
b. “…is reasonably likely to…” This is not so much a problem of definition as it is a problem of determination. If you want something concrete, the default definition could be “provides at least a 10% chance of,” adjusted as necessary (i.e., use a bigger number for a more burdensome intervention). In most cases, there is no consistent or agreed-on approach to deciding the likelihood of benefit from a particular procedure or medication or plan. Doctors make their estimates based on experience (and personal world view). However, the situation is not as hopeless as this might suggest. If in doubt, it’s often possible to give a time-limited trial (say, 12 hours or 48 hours, depending on the predicted response trajectory) and then withdraw the intervention if there’s no satisfactory response by the agreed-on deadline. (I know it’s not as simple as I’ve presented, but this at least provides a strategy.)
c. Here’s some additional guidance for specific situations:
i. If I have metastatic cancer, a large stroke, advancing dementia, or another condition with poor chance of survival, I want only comfort care. (If I wake up, I can always countermand this instruction then, if I choose.)
ii. I want artificial nutrition and hydration only if they’re “reasonably likely to help” (see above) or if they are required to optimize comfort (which is rarely the case). To be more specific, if I have been persistently unconscious for more than a week with little prospect of recovery, I do not want enteral or parenteral nutrition or hydration started or continued. (This can be used as a guide for other situations that are similar to but not exactly like this.)
This may seem a bit gruesome, but it actually feels liberating to me, and I hope it’s not too discomfiting for you. Let me know if you have questions. Maybe next time I’ll talk about my wishes regarding funeral plans. (I wonder if Father Patrick will allow fireworks in the nave.)
Love,
Dad
Related Content About Advance Care Planning
- S1E09: Advance Directives
- Advance Directives – a firsthand account
- S1E28: Organ Donation
- S4E13: How to Protect Last Wishes for LGBTQ+ Individuals: a Guide for Advance Planning with Ezra Salter
- S1E21: Artificial Food and Fluids
- Search our site for content on funerals and burial options that interests you
End-of-Life Planning References:
- I Asked My Mom if She Was Prepared to Die – The New York Times (nytimes.com)
- 19 Evidence-Based Benefits of Advance Care Planning (acpdecisions.org)
- With End-of-Life Preparedness, Actions Speak Louder Than Words, Ethos Survey Finds (prnewswire.com)
Advance Directive Resources:
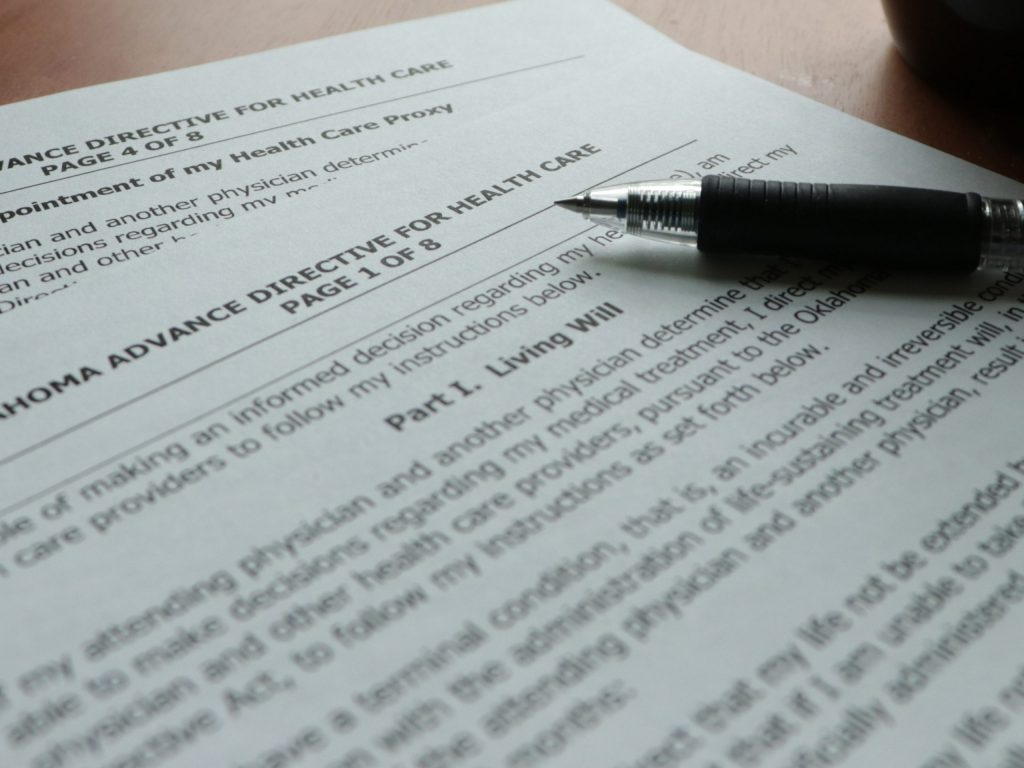
Advance Directives
- Instructions given by a patient while they still have decisional capacity concerning medical treatment they would or would not want.
- Formal advance directives typically consist of either a living will or a written health care proxy.
Durable power of attorney for health care
- A legal document that an individual signs, while competent, to designate who will make their healthcare decisions if they become incompetent (e.g. comatose, confused).
Other Links:
- State-by-State Advance Directive Forms – AARP
- Seven Ponds After Death Planning Guide
- Types of Advance Directives – American Cancer Society
- The Last Word – The Hospice Heart
Overlooked No More: Cordell Jackson
We share the story of an underappreciated rock legend – Cordell Jackson (1923-2004) – featured in the NY Times Overlooked No More segment. She started playing guitar when it wasn’t fashionable for women to do so, and forged a rock sound that predated many of the legends we associate with it by years.
Here are a couple more of Cordell Jackson’s performances:
- Late Show with David Letterman in the 1980s: YouTube
- With Brooklyn’s A-Bones backing her up. Miriam Linna on drums and Marcus Natale on bass. December 11, 1989, followed by a brief interview. (YouTube)
Recipe of the Week
What better way to herald spring than with a bit of sunshine? These lemon cloud cookies are perfect for your next get-together. Head to The Kitchn for the recipe.

Our Sponsors:
This episode was sponsored by The Tree of Life Memorials and Digital & Stone – a new platform to create digital memorials, environmental legacies and fine art monuments. Share the Stories, preserve the memories, conserve the land, connect the Souls…. because Love never dies. Find out more at https://www.digitalandstone.com/


https://blog.feedspot.com/palliative_care_podcasts/
Everyone Dies: and yes, it is normal!
Everyone Dies (and yes, it is normal) is a story about a young boy named Jax who finds something special on the beach where he and his grandpa Pops are enjoying a wonderful day. Pops helps Jax understand that death is a normal part of life. This book provides an age appropriate, non-scary, comfortable way to introduce the important topic of mortality to a preschool child. Its simple explanation will last a lifetime. Autographed copies for sale at: www.everyonediesthebook.com. Also available at Amazon
Mourning Jewelry

We offer a way to memorialize your loved one or treasured pet with a piece of handmade jewelry. When people comment on it and the wearer can say for example “I received this when my mother died” which opens the conversation about this loss. All our jewelry is made with semi-precious stones and beads, vintage beads, and pearls. You can choose between earrings or bracelets and the color family. Learn More