What do you do when frontline chemotherapy fails to stop cancer from growing? Your care team may offer the decision between aggressive anticancer treatment or palliative and hospice care. We share the story of one patient as she determined what was most important to her with the help of her multidisciplinary care team.
Jamie’s Story
In this episode, Marianne shared Jaime’s experience with non-small cell lung cancer. The first chemotherapy drug given is called first-line therapy, and for Jaime that was pemetrexed and cisplatin. She had four cycles but became so sick she needed to be hospitalized. After the fourth cycle, tests confirmed that the cancer had not responded to treatment.
Do I continue with a different treatment?
For second-line therapy, Jaime’s oncologist wanted her to start on immunotherapy medication, nivolumab. Another provider recommends she stop curative treatment and seek hospice care. Does she choose aggressive anticancer treatment or palliative and hospice care? At a palliative care consultation, Jaime wants to know whether this new treatment can provide the cure she and her family so desperately want. She also has to weigh side effects of treatment and other concerns.

“At this point in my life I just want time with my family. My youngest son is getting married in two months. I want to be there.”
As is true for many people with a new diagnosis of cancer, Jaime has gone through a rapid succession of tests and treatments and hasn’t considered her own needs and goals of care. When I ask her what her goals are, Jaime cries and says, “At this point in my life I just want time with my family. My youngest son is getting married in two months. I want to be there.”
Is there a cost-benefit with cancer treatment?
A study by the American Society of Clinical Oncology (ASCO) found that a cancer diagnosis almost triples the likelihood of bankruptcy. According to a study published in Cancer Epidemiology, Biomarkers & Prevention (2020), the annual costs for cancer-related medical services and drugs are projected to total nearly $246 billion nationally in 2030. This figure corresponds to a 34% increase in national costs since 2015. These cost estimates include cancer-attributable costs for medical services and oral prescription drugs. These national cancer medical care costs are substantial and projected to increase dramatically by 2030, reflecting the rising burden of cancer care among cancer survivors.
Most people believe that they “get what they pay for,” yet findings from cost–benefit analyses have shown no correlation between the price of chemotherapeutic drugs and measures such as survival time and quality of life.
Nivolumab has a yearly cost of $187,000 ($7194. every other week), is not curative for lung cancer, and on average offers patients an additional 3.2 months of life. 20% of people will survive one year on this medication (and 80% will not).
Still, despite the costs and risks, some patients with advanced cancer understandably want to try expensive drugs like a PD-1 inhibitor in the hope that it might help “beating a cancer death sentence,” — or more accurately, extend their progression-free survival time.
Are there any advantages to hospice care?
The other option Jaime was offered was Hospice support (see resources for past shows and info on eligibility.)
Obermeyer and colleagues compared two groups of patients with advanced cancers: those receiving hospice care and those not. They concluded that those receiving hospice care had significantly lower rates of hospitalization, decreased use of intensive care interventions, and significantly lower total costs in the last year of life.
Determining Priorities – A Family Meeting with the Care Team
Jaime was struggling with her decision, and so we arranged for a family meeting with her medical team, plus a hospice nurse. At the meeting Jaime shared her goals, and the team discussed how each would be supported by her options: aggressive treatment or hospice care.
Jaime does not want to return to the hospital, she says, but deciding to stop curative treatment means she’ll need supportive care for any symptoms that arise as a result. During the discussion Jaime appears to be asking her oncologist for permission to discontinue aggressive treatment. In fact, research has shown that conversations about end-of-life care are most effective when they’re held with a physician the patient trusts.
Jaime decides that she wants to receive hospice care at home. The family meeting includes a discussion of advance directives, and all forms are completed. (See below for podcasts related to this topic.)
Weigh the Risks and Benefits
So how can you help family, friends, or even yourself when faced with the choice between aggressive, potentially burdensome treatments and hospice care—especially if palliative care teams are not available?
Understand the risks and benefits of the approaches being offered are vital and questions that you should ask both the oncologist and your primary medical practitioner. Try to help identify the personal values and goals that guide care choices. Encouraging the discussion of individual interpretations of treatments offered is vital. A simple question such as “What did the physician tell you?” can start a conversation that can help answer the above questions and start you on the road to making this important decision.
Be sure to listen to the podcast for the full story and discussion!
Related Podcasts:
- S2E29: How do you decide if it is time for hospice care?
- S1E30: The Expectations of Hospice Care
- S1E18: Hospice and End of Life with Mary Kazanowski
- S1E09: Advance Directives
References:
- Collins, R., & Matzo, M. (2016). For Advanced Cancer, What Treatment Is Next?. The American journal of nursing, 116(10), 50–53. https://doi.org/10.1097/01.NAJ.0000503302.07015.7d
- Matzo, M. Palliative Chemotherapy. AJN, American Journal of Nursing 116(6):p 59-62, June 2016. | DOI: 10.1097/01.NAJ.0000484234.39869.cd
- Committee on Approaching Death: Addressing Key End-ofLife Issues, Institute of Medicine of the National Academies. Dying in America: improving quality and honoring individual preferences near the end of life. Washington, DC: National Academies Press; 2015. http://www.nap.edu/catalog/18748/ dying-in-America-improving-quality-and-honoring-individualpreferences-near.
- Mariotto, A. B., Enewold, L., Zhao, J., Zeruto, C. A., & Yabroff, K. R. (2020). Medical Care Costs Associated with Cancer Survivorship in the United States. Cancer epidemiology, biomarkers & preventio: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology, 29(7), 1304–1312. https://doi.org/10.1158/1055-9965.EPI-19-1534. Medical Care Costs Associated with Cancer Survivorship in the United States (silverchair.com)
- Cost & Pricing Information | OPDIVO® (nivolumab) and OPDIVO-based Combinations (bmspricinginformation.com)
- Obermeyer Z, et al. Physician characteristics strongly predict patient enrollment in hospice. Health Aff (Millwood) 2015; 34(6):993-1000
Resources:
Using the power of music at the end of life

Charlie shared with us about a Psychology Today article about music and how important it can be at the time of our final transition from this life to provide peace and comfort, not only to the dying but to family members as well. Research into the use of music in hospice and palliative care has consistently found that patients, family, and staff all benefit from the music, and often after only one session. Music has been found to help decrease anxiety, agitation, and pain. It also helps patients to slow and deepen their breath. You can read the whole article here!
Recipe of the Week
Go to any funeral lunch and you will likely see a table full of casseroles in Pyrex dishes. But are they casseroles or a hotdish? Hotdish, the unofficial state cuisine of Minnesota, is a comfort food staple found in households across the Upper Midwest. Incorporating a mixture of simple, thrifty ingredients and mix-it-together cooking techniques, it invokes a sense of nostalgia amongst fans. A creamy sauce binds three essential hotdish components together: starch, protein, and vegetable.
Tune in for a good laugh as we talk all about the culture, and be sure to watch the documentary below. Who knows, it might just give you some ideas of what to do with those cans lurking in the back of your pantry!


https://blog.feedspot.com/palliative_care_podcasts/
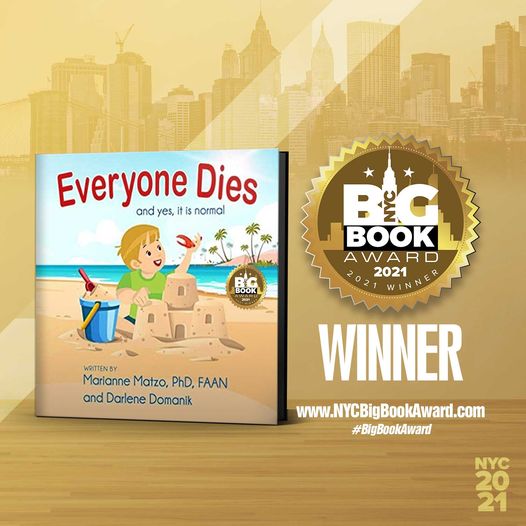
Everyone Dies: and yes, it is normal!
Everyone Dies (and yes, it is normal) is a story about a young boy named Jax who finds something special on the beach where he and his grandpa Pops are enjoying a wonderful day. Pops helps Jax understand that death is a normal part of life. This book provides an age appropriate, non-scary, comfortable way to introduce the important topic of mortality to a preschool child. Its simple explanation will last a lifetime. Autographed copies for sale at: www.everyonediesthebook.com. Also available at Amazon
Mourning Jewelry

We offer a way to memorialize your loved one or treasured pet with a piece of handmade jewelry. When people comment on it and the wearer can say for example “I received this when my mother died” which opens the conversation about this loss. All our jewelry is made with semi-precious stones and beads, vintage beads, and pearls. You can choose between earrings or bracelets and the color family. Learn More