Palliative chemotherapy is often offered for those with widely metastatic disease to ease symptoms, but does it accomplish its goals? Learn what the science says.
Is chemotherapy going to help me? And if it’s not, why are they offering it?
Now, this is a really good question! We assume that if we are diagnosed with cancer that chemotherapy or surgery or radiation is going to be offered to cure the disease. The things that are considered are the type of cancer, stage of disease, treatments available, general health of the person, and goals of care.
What is Palliative Chemotherapy?
Chemotherapy for people with widely metastatic disease has been offered for the last 25 years to palliate symptoms—hence its name, palliative chemotherapy. Palliative chemotherapy is treatment given “in circumstances where the impact of treatment is insufficient to result in major survival advantage, but does affect improvement in terms of tumor-related symptoms, and where the palliation/toxicity trade-off from treatment clearly favors symptom relief.”
The thinking is that by slowing tumor growth, shrinking tumor size, relieving pressure on nerves and organs, and controlling pain, the intervention could improve a patient’s quality of life.
Unfortunately, many patients and family members believe that they are still “fighting the cancer” with hope of a cure, and don’t understand the chemotherapy is only to try to help with symptoms, even when the doctor has explained it.

Is the Chemotherapy Worth the Tradeoff?
We share multiple studies that show that palliative chemotherapy prescribed in end-stage cancer did not improve survival and was significantly associated with worse quality of life near death.
A retrospective review of chemotherapy use in older adults (age over 60 years) with acute myeloid leukemia categorized people according to intensive chemotherapy and nonintensive chemotherapy. Eighty-eight percent of the people died during the study period, but only 16% received palliative care and 23% received hospice care. In the last 30 days of life, 84% were hospitalized and 61% died in the hospital.
Among the patients who died, those who received intensive chemotherapy spent 30% more of their life after diagnosis in the hospital and were less likely to receive hospice services than those receiving nonintensive chemotherapy.
We often discuss the benefits of early hospice to the individual and family, (S2E29: How do you decide if it is time for hospice care?; S1E18: Hospice and End of Life with Mary Kazanowski) and it is tragic that palliative chemotherapy reduced these important referrals and services.
“I like my independence.
– Brent, after Stage IV Lung Cancer Diagnosis
I like my little house in the country,
where I can be my own man,
live life on my own terms.”
What Do You Hope For?
We talk about Brent, age 59, whom Dr. Matzo met within days of his receiving a diagnosis of stage IV lung cancer. He had lost 50 lbs. in the three months prior, and tests revealed non–small cell lung cancer that had metastasized to his throat, spine, liver, and brain. The oncologist was offering palliative chemotherapy and a percutaneous endoscopic gastrostomy (PEG) tube to deliver nutrition. He was furious with his situation; he was too weak to return to his rural home where he lived alone, but did not want to stay in the hospital. His medical team was waiting for him to decide about the treatment they were offering.

When Marianne asked Brent what he hoped for at that point in his life. “I like my independence,” he said. “I like my little house in the country, where I can be my own man, live life on my own terms.” He showed me pictures of his golden retriever and talked about wanting to care for her. As he talked through his options, he said he couldn’t see how coming to the infusion center from his rural home made any sense.
Fortunately for Brent, his longtime neighbor offered to help care for him at home so that he could receive hospice services. Mr. Brigham declined both chemotherapy and the PEG tube and returned home to his dog.
Making an Educated Choice
The American Society of Clinical Oncology (ASCO) has published recommendations stating that further chemotherapy has no clinical value to patients in whom it has failed, who have an ECOG score of 3 or more, and who have been diagnosed with a solid tumor (e.g. not a cancer in the blood such as leukemia).
The ASCO expert panel notes that in patients for whom chemotherapy offers no evidence of clinical value, it’s nonetheless commonly used. The panel stated that many patients are unprepared for high out-of-pocket costs of treatment, especially in light of its benefit in extending life by only days or weeks, if at all.
So what is ECOG?
The ECOG is a scale developed by the Eastern Cooperative Oncology Group (ECOG) to create standard criteria for measuring how the disease impacts a patient’s daily living abilities, known to physicians and researchers as a patient’s performance status. It describes a patient’s level of functioning in terms of their ability to care for themself, daily activity, and physical ability (walking, working, etc.).
| Grade | ECOG Performance Status |
|---|---|
| 0 | Fully active, able to carry on all pre-disease performance without restriction |
| 1 | Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, e.g., light house work, office work |
| 2 | Ambulatory and capable of all selfcare but unable to carry out any work activities; up and about more than 50% of waking hours |
| 3 | Capable of only limited selfcare; confined to bed or chair more than 50% of waking hours |
| 4 | Completely disabled; cannot carry on any selfcare; totally confined to bed or chair |
| 5 | Dead |
Findings from the studies we’ve cited, among others, show the low use of palliative care and hospice services and the widespread use of chemotherapy despite potential harm in patients with progressive metastatic disease. In working with other nurses and with patients and families, we have seen that quality of life at the end of life often begins with clinicians’ willingness to deal with patients’ distress in facing a life-limiting disease.
If palliative care – which focuses on relieving symptoms and providing support to patients and families – was not offered at the time of a cancer diagnosis, then it most certainly should be offered when palliative chemotherapy is being considered. Many nurses and physicians never initiate these difficult conversations. If you or a loved one are facing progressive metastatic disease, don’t be afraid to be the one to bring it up and request a palliative care consult!
Related Episodes:
- S2E29: How do you decide if it is time for hospice care?
- S1E18: Hospice and End of Life with Mary Kazanowski
- S1E30: The Expectations of Hospice Care
- S3E12: Pleasures at the End of Life
References:
- Collins, R., & Matzo, M. (2016). For Advanced Cancer, What Treatment Is Next?. The American journal of nursing, 116(10), 50–53. https://doi.org/10.1097/01.NAJ.0000503302.07015.7d
- Matzo, M. Palliative Chemotherapy. AJN, American Journal of Nursing 116(6):p 59-62, June 2016. | DOI: 10.1097/01.NAJ.0000484234.39869.cd
- Committee on Approaching Death: Addressing Key End-ofLife Issues, Institute of Medicine of the National Academies. Dying in America: improving quality and honoring individual preferences near the end of life. Washington, DC: National Academies Press; 2015. http://www.nap.edu/catalog/18748/ dying-in-America-improving-quality-and-honoring-individualpreferences-near.
I have terminal cancer. A houseplant is helping me confront mortality.

Charlie read an essay written by David Meyers who is a family physician and a health policy researcher in the Washington, D.C. area and living with terminal cancer. You can read the full article in Washington Post here.
Humor at the End of Life
We talked about the role of humor for serious illness and end of life. We get mixed reactions (and lots of comments!) about our use of humor in our podcast. But there is solid evidence about its role and how it is vital for those going through any kind of difficult situation. According to one study published in the American Journal of Hospice and Palliative Medicine, laughter and humor can fulfill one of the main goals of hospice palliative care, which is the improvement of a patient’s overall quality of life. You can read more facts here (Pathways Health). And as promised, here is the link to the Chicago tribute article Using Humor to Aid the Dying (Laughing in the Face of Death).
Recipe of the Week
We bring you Honey Tea Cake Loaf this week from Lifestyle of a Foodie. This honey tea cake is moist, dense and perfect for an afternoon treat or your next funeral lunch.

https://blog.feedspot.com/palliative_care_podcasts/

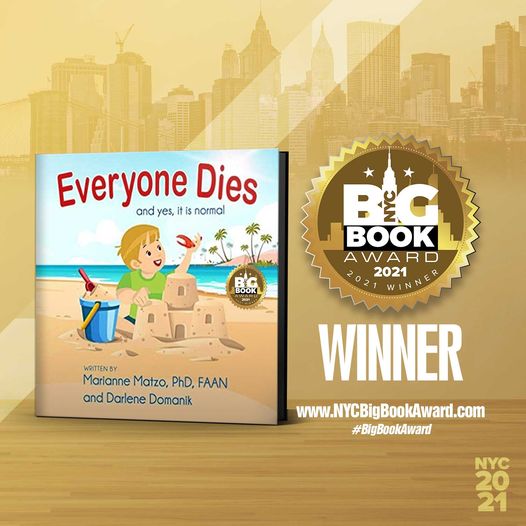
Everyone Dies: and yes, it is normal!
Everyone Dies (and yes, it is normal) is a story about a young boy named Jax who finds something special on the beach where he and his grandpa Pops are enjoying a wonderful day. Pops helps Jax understand that death is a normal part of life. This book provides an age appropriate, non-scary, comfortable way to introduce the important topic of mortality to a preschool child. Its simple explanation will last a lifetime. Autographed copies for sale at: www.everyonediesthebook.com. Also available at Amazon
Mourning Jewelry

We offer a way to memorialize your loved one or treasured pet with a piece of handmade jewelry. When people comment on it and the wearer can say for example “I received this when my mother died” which opens the conversation about this loss. All our jewelry is made with semi-precious stones and beads, vintage beads, and pearls. You can choose between earrings or bracelets and the color family. Learn More